Our Facility
Our facility is equipped with the latest equipment to conduct tests on bacteria, bacteriophages, mycobacteria, yeast, fungi, viruses and bacterial spores.
All our tests are carried out in one of the 3 laboratories at Viroxy and they are fully equipped to meet the challenges of microbiological testing. At the moment, we have a microbiology laboratory, a tissue culture laboratory and a virology laboratory with plans to include physical and chemical testing laboratories in the near future.
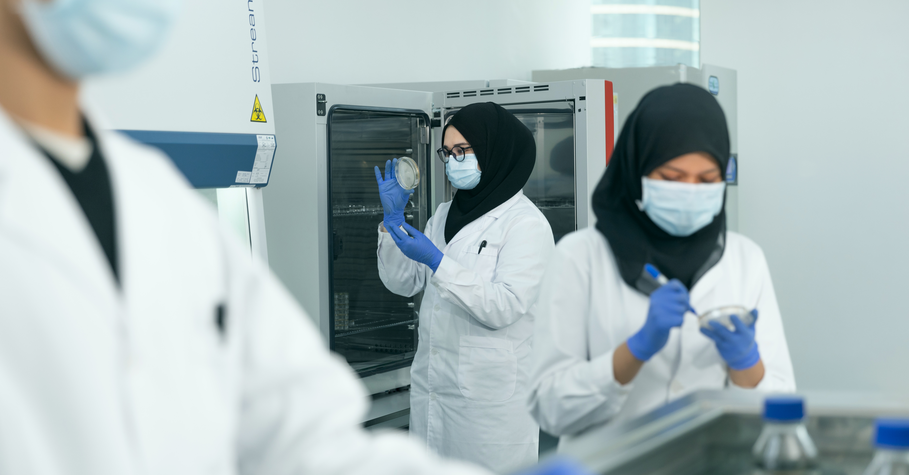
Microbiology Laboratory
Our microbiologists spend a considerable amount of time in the microbiology laboratory either preparing for or conducting tests. Their typical day at work includes:
Culture preparation – Each strain of test bacteria is combined with a cryoprotectant in separate containers and stored in an ultra-low temperature freezer. This is to prolong the lifespan of test microorganisms and make them available as and when a test needs to be conducted. When done correctly, each culture can last up to 5 years.
Microbiological sample preparation – When a test request is received, the required microorganism or bacterial strain is retrieved from the ultra-low temperature freezer and revived. The process includes dipping a sterile inoculating loop into a bacterial culture and streaking the loop across a fresh agar plate for cultivation. This process is repeated twice more at one day intervals, transferring portions of the culture into a new plate successively until a sample that is suitable for testing is acquired.
Media preparation – This refers to the agar plates used to cultivate bacteria either before or while a test is in progress. Although preparing a plate full of agar may sound easy enough, the actual process is a bit more complex than boiling a bowl of Jell-O at home. Firstly, the media has to be sterile to avoid pre-test contamination and as such must be autoclaved. Secondly, it must be maintained at a suitable pH value and contain appropriate nutrients to aid the proliferation of bacteria when a test is being carried out.
Disinfectant efficacy testing – Once the above items and the appropriate reagents are ready, suspension and carrier tests can be performed according to specified standards.
Suspension test – In a suspension test, bacterial culture such as Pseudomonas Aeruginosa is suspended into disinfectant solution. A neutraliser is added immediately after the contact time to prevent continued disinfection and a subculture of the solution is analysed to verify if the microorganism is killed. In a qualitative suspension test, the result is expressed as ‘growth’ or ‘no growth’ while in a quantitative suspension test, the number of surviving microorganism is counted and compared to the original culture size.
Carrier test – A piece of sterile glass, wood or metal acts as a ‘disease’ carrier and as such is contaminated with a liquid culture of test microorganism. The carrier is left to dry to simulate actual conditions and submerged in disinfectant for the duration of contact time before it is submerged in a neutraliser. A sample of the solution is poured into pour plates and cultured in nutrient medium and incubated. If no bacterial growth is detected, the disinfectant is deemed as successful at killing the test microorganism.

Tissue Culture Laboratory
Tissue culture is the fascinating process of growing tissue cells separate from the organism for laboratory testing and research. At Viroxy, tissue cultures form an integral part of tests conducted at our virology laboratory. As each cell line is cultured differently, let’s take HeLa, one of the oldest and most famous cell lines among research community as an example to understand what really goes on in this laboratory.
Henrietta Lacks, a poor farmer, died of cervical cancer in October 1951. Her tumour cells were taken and named HeLa, representing the first two letters of her first and last name. It is the most commonly used cell line in testing laboratories due to its resilience and naturally ‘immortal’ characteristic. Later, the cell line became instrumental in the development of polio vaccine, in-vitro fertilisation, cloning and many other scientific achievements. Today, these immortal cells continue to be widely used in testing laboratories around the world.
HeLa cells are cultured in flasks in liquid suspension containing nutrients and incubated at 37°C with 5% CO2. At these optimal conditions, the cells multiply and grow by adhering to the bottom of the flask. When the cells reach 90% confluence, trypsin is added into the flask to break the protein bonds and float the cells to the surface. Once the cells are released, a subculture is prepared, counted and transferred to a fresh medium in a smaller number to continue multiplying. This is known as subculturing or passaging the cells.
If a cell line is cultured for long term storage, it is frozen gradually in liquid nitrogen to avoid cell crystallisation. When required for testing, the cell line is defrosted rapidly in a water bath and replaced in a nutrient medium. Several rounds of passage are required before the cell line can return to normal. Next, the culture is transferred into a 96-well plate to continue multiplying. Once the entire surface of the plate is covered in cell growth, it is placed in a pass box and shifted to virology laboratory.

Virology Laboratory
Viruses are small, non-living, infectious agents that can only replicate inside the living cells of other organisms known as hosts. Without a host cell, viruses cannot perform life-sustaining functions or reproduce. Viruses can be subdivided to enveloped and non-enveloped types with the non-enveloped being more resistant. Both classes of virus can infect all living organisms including animals, plants and even bacteria. And unlike bacteria, viruses do not form colonies and as such are visible neither to the naked eyes nor through a light microscope. Most are smaller than bacteria and can only be seen through an electron microscope. Typically, the presence of a virus is only ‘indirectly detected’ when cytopathic effect (CPE) or the death of host cell is observed. For this reason, cell culture is the most common method used for the propagation of viruses in disinfectant efficacy testing.
Once a cell culture is ready, a virus strain is introduced and incubated in appropriate conditions depending on the virus being tested. The culture is then examined daily with an inverted microscope for signs of CPE. Healthy cells grow by adhering to the bottom of the culture flask and a CPE cannot be detected. If a disinfectant is unsuccessful in deactivating the test virus, the host cells change shape, become more refractive and signs of CPE will be visible. Some infected cells may even detach from the culture flask and float in the medium.
At Viroxy, we conduct tests on viruses according to EN 14476 and EN 14675. According to the European Norms, it is sufficient for a disinfectant to demonstrate the ability to inactivate three particular non-enveloped viruses i.e. poliovirus, adenovirus and norovirus to prove efficacy against all viruses as they are more resilient compared to enveloped viruses.
Tests conducted on viruses require extra precaution compared to other tests as it is easier to contaminate a cell culture with just the slightest technical error. Each test involves multiple controls and it must be conducted in aseptic conditions. As a result, virology laboratories require high maintenance to preserve the purity of the environment. Our virologists change their shoes, mop and disinfect every surface after each test as viruses can linger in the air and remain stable on bench tops for months.

